FACULTY MEMBERS IN THE TELENEUROLOGY SECTION ARE LEADING RESEARCH IN THE FOLLOWING AREAS:
C3FIT – Coordinated, Collaborative, Comprehensive, Family-focused, Integrated, Technology-Enabled to Improve Stroke Care
Patient support after stroke requires a long-term commitment, supporting the patient as they move through “nodes” of acute care, post-acute in-hospital care, subacute care (inpatient rehab, extended stay, etc.), and chronic care. The current standard of stroke care is the Joint Commission (JC)-certified Comprehensive Stroke Center or Primary Stroke Center (CSC/PSC) care system, a collection of proven processes of care, but an approach with a focus on acute care (and to a lesser extent the post-acute in-hospital care), with little coordination of care of the patient after discharge. The overall goal of C3FIT is to assess if patient outcomes are improved when the CSC/PSC system is supplemented with an Integrated Stroke Practice Unit (ISPU) system of care, a patient-centric model of care involving the patient’s caregiver that coordinates care from the acute management through the rehabilitation and recovery of the patient.
Integrated Stroke Practice Unit: The ISPU is an innovative care model that builds on the JC-certified CSC/PSC design by increasing coordination of care using a patient/caregiver-centric design. C3FIT’s ISPU two coordinated units, Stroke Central and Stroke Mobile, are connected by a technology-enabled coordinating bridge, Stroke Connect that addresses the entire care continuum for the patient, from acute through hospital care to 1-year post-discharge care. Stroke Central and Stroke Mobile can be thought of as components of Stroke Connect
C3Fit Clinical Sites
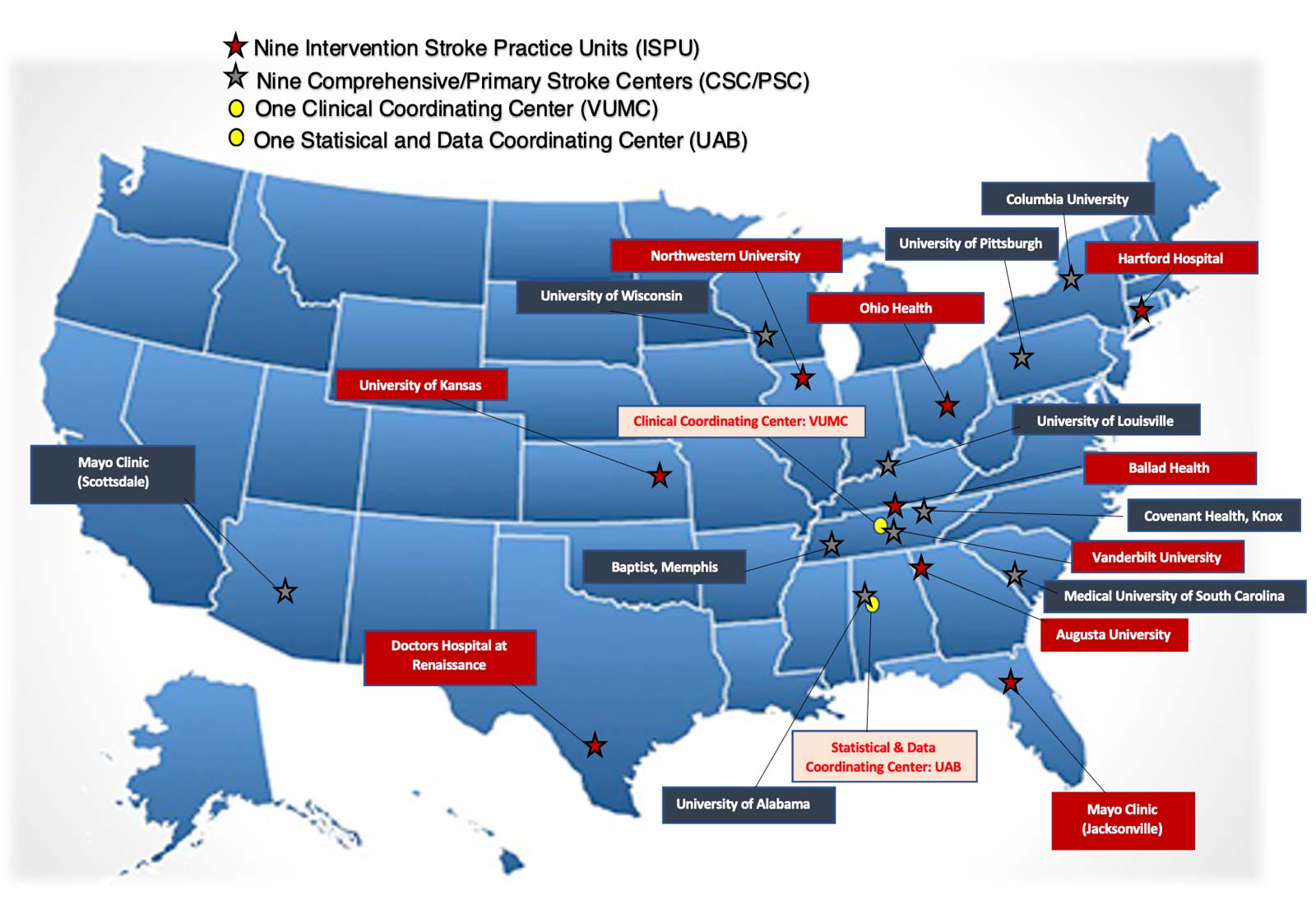
The specific aim of this project is to assess superiority of patient-centric outcomes between the CSC/PSC and ISPU models in a cluster-randomized pragmatic trial conducted at approximately 18 clinical sites in the United States (US). The primary aim focuses on differences in 12-months post stroke quality of life (QOL) using the Stroke Impact Scale (SIS) and patient function using the Modified Rankin Scale (mRS). Secondary aims include other patient/caregiver-centered outcomes, including: (1) short-term function and QOL using the SIS and mRS; (2) longer-term durability of CSC/PSC-versus-ISPU intervention differences using SIS and mRS; (3) control of stroke risk factors; (4) mortality, recurrent stroke rates, and hospital readmission rates; (5) Time At Home; (6) patient depression, using the Patient Health Questionnaire (PHQ-9); and (7) caregiver strain, using the Caregiver Strain Index (CSI). Finally, we aim to determine whether there are patient subgroups specifically responsive or resilient to the intervention, according to effect modification by age, race, sex, and socio-economic status (income and education).
C3FIT is a multicenter, randomized, single blinded, Phase III, cluster randomized trial. Sites will be stratified by patient admission volume and geographic location; subsequently, each site will be randomized to one of two patient care management strategies: the CSC/PSC versus ISPU model. C3FIT’s primary outcomes are the SIS and mRS at 12 months. Based on the primary outcome, the study is designed for a total sample size of approximately 1800 patients, with approximately 18 sites, each enrolling approximately 100 patients. The target is 900 patients in each intervention arm.
Interventions. Coordinated care (including in-home/in-patient rehabilitation and skilled nursing or extended care facility visits) will be provided based on protocol-based coordination of post-acute in-home/facility care for ISPU Site patients, while CSC/PSC patients will be managed per standard CSC/PSC protocol with no additional study related management post discharge. The clinical sites have been provided training specific to the arm to which they are randomized. Patients are followed at the site level for one year after enrollment. Two years after enrollment, patients will be reassessed centrally by the University of Alabama at Birmingham’s (UAB) Statistical and Data Coordinating Center (SDCC) to determine the durability of intervention effects.
This study is registered at www.clinicaltrials.gov; the ClinicalTrials.gov identifier is NCT04000971.
USDA Distance Learning & Telemedicine Grant
Emergency Medical Service (EMS) staff provide a critical first step to improving timely assessment and diagnosis for stroke, as well as accurate medical information to Emergency Department (ED) providers, including symptom start time, medical history, and demographic information that can be beneficial in acute care treatment. Paramedic stroke recognition and hospital pre-notification of stroke are significantly associated with shorter times from ambulance call to first medical assessment, door-to-computerized tomography (CT) scan performance; further, these factors double the rate of thrombolytic therapy given to patients. Unfortunately, identifying mild and non-specific strokes can be particularly difficult even in the ED, but insufficient research has been conducted to assess the misdiagnosis rate in the EMS setting.
This feasibility project, funded in part through a United States Department of Agriculture (USDA) 2017 Distance Learning and Telemedicine (DLT) award, will utilize audio/video-enabled telemedicine technology to connect EMS/Ambulance Service personnel in the field in Jackson, Overton, and Pickett Counties’ (End-User Sites) with specialty-trained personnel housed at Livingston Regional Hospital (Hub Site) in rural northeastern Tennessee. The project will address issues in assessment and diagnosis at a key point in acute stroke care for the patient: during transport by EMS personnel. It will meet two key needs in prehospital care for stroke:
- Providing access to stroke-trained personnel in rural areas where specialty care is often limited.
- Enhanced acute stroke evaluation, diagnosis, and management in the field will increase timeliness of EMS response, accuracy of diagnosis, and timely thrombolytic therapy and interventional treatment in the prehospital phase.
We will determine the feasibility of developing a rural telemedicine network for prehospital stroke assessment and diagnosis in specific counties in Tennessee that connects stroke-trained personnel located at Livingston Regional Hospital (Hub Site) with EMS ambulances (Spoke Sites) in rural Tennessee counties. Developing telemedicine linkages to stroke-trained personnel will provide needed expertise for stroke assessment and diagnosis that is not currently integrated into prehospital care for stroke. Informal communication with EMS personnel in this region suggests that they would find additional diagnostic assistance from someone specially trained in stroke would be helpful in making a more definitive stroke diagnosis and in helping to determine the most appropriate hospital and transport option for patients whose stroke has been more clearly delineated. Further, enhanced acute stroke evaluation, diagnosis, and management in the field will increase timeliness of EMS response, accuracy of diagnosis, and timely thrombolytic therapy and interventional treatment in the prehospital phase, which will lead to improved outcomes for stroke patients.