Sleep Disorders
Disorders of sleep and wakefulness affect some 70 million Americans, making them among the most common medical conditions. There are thought to be 85 different categories of sleep disturbances, but two — insomnia and sleep apnea — are the most common and important for public health. Surprisingly, perhaps, about 25 percent of American children between one to five years of age have a sleep disturbance. An estimated 250,000 people suffer from narcolepsy. More than half of Americans aged 65 and older have a sleep problem, and disturbed sleep is among the reasons most frequently cited by caretakers for institutionalization of older people.
What is sleep? Why do we need it?
It would be much easier to do research in sleep if we had an understanding of why we need it, but the best answer available to why we sleep at night is so we won't be sleepy during the day and also to reset our brains so we are able to think more clearly and keep our emotions in check. Sleep is a universal trait of mammals and birds, and may be related to being warm-blooded. The length of sleep varies throughout the animal kingdom, and many species have evolved interesting ways of protecting themselves while sleeping. Dolphins, for example, appear to have microsleeps, where only one hemisphere of the brain at a time shuts down. The common experience of fatigue, sleepiness, and irritability that results from a poor night of sleep teaches us that sleep is a requirement that may be temporarily foresworn, but cannot be permanently ignored. Sleep restriction experiments have shown that eventually everyone will fall asleep.
Physiology of Sleep
Although we cannot explain why we sleep, we have learned quite a bit about how we do it. Sleep is not a passive process, but has complex control mechanisms that produce characteristic sleep patterns each night, and bring us to sleep at defined intervals. Volunteers living in a cave in total darkness with no visual, temperature, or auditory clues have a regular sleep-wake cycle, although it is slightly longer than our usual cycle because they lack light clues. That part of the sleep control mechanism is not available to our conscious control, so although you can allow yourself to go to sleep, you cannot consciously force yourself to go to sleep.
By using surface electrodes, brain waves can be recorded during sleep, revealing characteristic patterns that follow one another in regular fashion throughout a night of sleep. In stage N1, the lightest stage of sleep, one can still attend to the outside world. Stage N2 is a deeper sleep, and is usually followed by slow wave sleep (Stage N3) during which is harder to arouse. It is in these later stages when sleep walking and night terrors occur. Rapid eye movement sleep (REM) has a radically different EEG pattern; in fact, the brain wave patterns are characteristic of a person awake. During REM the skeletal muscles are paralyzed, and it is then that most dreams occur. This sequence of stages of sleep repeats itself several times throughout the night.
Sleep Apnea
The periodic obstruction of the airway during sleep by the tongue and soft tissues is a common sleep disorder, with serious consequences. Each year, sleep apnea accounts for about $42 million in hospital bills. It has been estimated that as many as 18 million Americans have sleep apnea. Approximately four percent of middle-aged men and two percent of middle-aged women have sleep apnea along with excessive daytime sleepiness.
Sleep apnea requires an anatomic and a central nervous system predisposition. One doesn't have apnea unless one is asleep, and alcohol and sedatives make it worse. The anatomy of the airway is critical, and any narrowing of the upper airway, whether by fat (yes, one gets fat there too), tonsils, or allergic rhinitis, makes apnea worse.
To restore breathing, patients may awaken briefly and move the tongue out of the back of the throat. Since apnea may happen every two minutes or more during the night, the resulting sleep deprivation is devastating. In fact, the most important diagnostic criterion for sleep apnea is excessive daytime sleepiness. Measures of daytime sleepiness, such as the multiple sleep latency test, are valuable but imperfect, since conscious effort can overcome much sleepiness.
The Epworth sleepiness scale is one simple index of sleepiness:
Chances of dosing: 0 - Never, 1 - slight 2 - Moderate, 3 - High
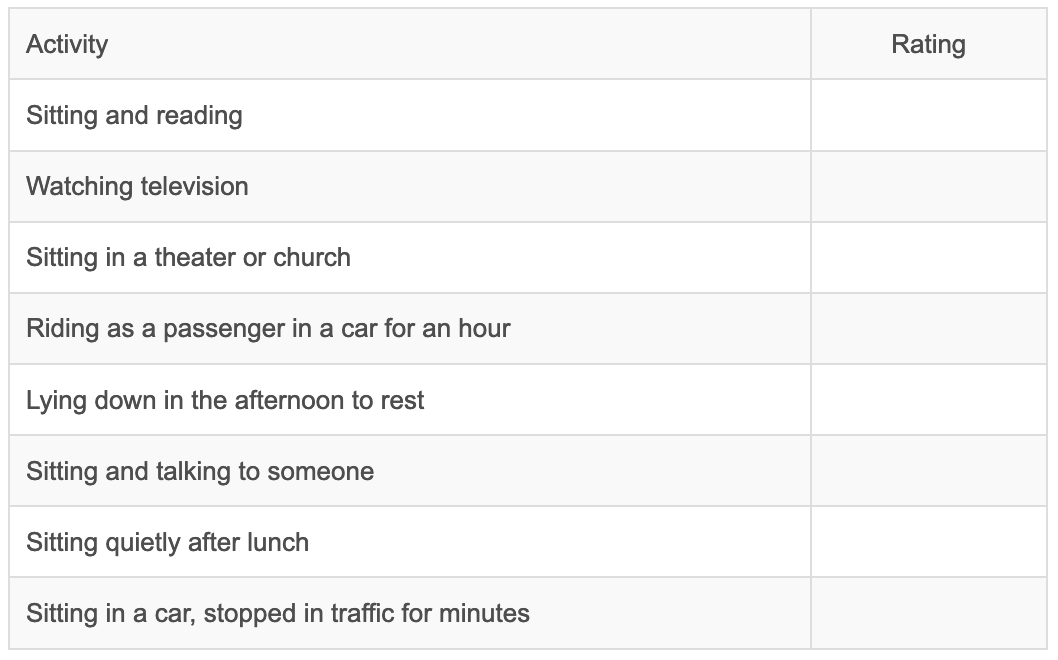
Although imprecise, the scores of 9-12 indicate a mild degree of sleepiness, 13-18 a moderate degree, and above that a severe degree of sleepiness. The scores correlate roughly with the number of apneic episodes occurring each hour of sleep. You can take this test online at the National Sleep Foundation site: http://www.sleepfoundation.org/epworth/quiz.html
The diagnosis of sleep apnea is suggested in people who snore, may have had apnea witnessed, and are sleepy during the day despite what should be adequate sleep time at night. It is confirmed during the course of an overnight sleep study (nocturnal polysomnography) where sleep stages, arousals, breathing, oxygenation, electrocardiogram, and leg movements are monitored. The only 100% effective therapy is continuous positive airway pressure (CPAP), customarily applied via a nasal mask. Surgical correction of anatomic abnormalities can help, as can dental devices. Weight loss may be beneficial.
Insomnia
The inability to fall asleep and stay asleep is a common experience. Anxiety about upcoming events is usually the cause, and the insomnia usually abates when the event is over. Hypnotic sedatives can be of use in this situation, but because they are associated with tolerance and addiction they are usually not long-term solutions. In some unfortunate people, the insomnia becomes chronic; at that point, psychological counseling, behavioral techniques and perhaps pharmacotherapy can be beneficial. Help for depression and other medical conditions should be sought.
Insomnia Quiz: Circle those statements that describe any symptoms you have had in the past year.
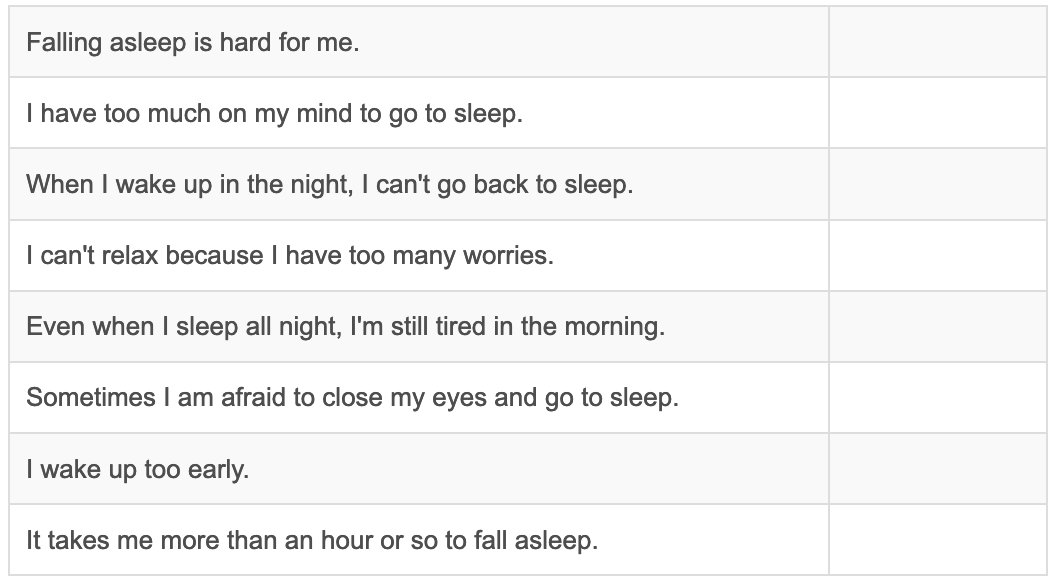
Rarely does insomnia require an overnight sleep study, and then it is done not to diagnose insomnia but to rule out other problems. The sleep of patients with insomnia is characteristically better when they are in an unusual environment, and is better than they report. Patients with insomnia may feel awful and very sleepy, but they do not fall asleep easily or often during the day, and their Epworth sleepiness scores are usually normal.
Everyone could benefit from the rules of good sleep given below by your grandmother (or in this case, the National Sleep Advisory Council). Patients with insomnia must abide by them if they are to improve.
- Go to bed at the same time each evening, and get up at the same time. (This allows the brain’s internal clock to aid in allowing one to go to sleep, and to get up.)
- Don't eat or exercise within three hours of going to bed.
- Have a comfortable, quiet, dark sleeping arrangement.
- Don't read or watch TV in the bed.
- Don't nap during the day. (This restriction may be relaxed in some patients, but the nap should never be longer than an hour.)
- Don't drink caffeine or alcohol within 3 hours of going to sleep.
Narcolepsy
This inheritable disease of the central nervous system characteristically manifests itself with overwhelming urges to sleep during the day, bad dreams at sleep onset, and sudden attacks of weakness brought on by emotion. Its onset occurs in adolescence, and it becomes a lifelong problem. Although it is estimated that narcolepsy afflicts as many as 200,000 Americans, fewer than 50,000 are diagnosed. It is as widespread as Parkinson's disease or multiple sclerosis, and more prevalent than cystic fibrosis, yet it is less well known. Recent evidence from studies in mice, dogs, and humans suggests that it may be caused by a deficit in a neural protein, hypocretin. This finding offers the first possibility of designing a drug to specifically target narcolepsy. After ruling out sleep deprivation with an overnight sleep study, a multiple sleep latency test is done during the following day. Narcoleptics will have short sleep latencies and develop early onset of REM sleep. One explanation of their disease is that they have intrusion of REM sleep into the daytime, causing sleepiness and the characteristic transient paralysis known as cataplexy. The cataplexy can be treated with drugs such as tricyclic antidepressants, which suppress REM sleep. The sleepiness is treated with good sleep hygiene, scheduled naps, and central nervous system stimulants.
Restless Legs Syndrome
The irresistible urge to move legs and sometimes arms to alleviate unpleasant sensations in the muscles constitutes the restless leg syndrome. It is slightly more common in women than men, and may be inherited. It may be associated with muscle jerks during sleep, known as periodic limb movements of sleep. Insomnia and non-restorative sleep are common features of restless legs. Restless leg syndrome is common in pregnancy, dialysis, and in iron-deficient states. The diagnosis can be made by a physician knowledgeable in sleep disorders, and usually does not require special testing or sleep studies. Treatment with medicines used for Parkinson’s disease, sedatives, and narcotics can be helpful. More information is available at the Restless Legs Syndrome Foundation web site.
Website References:
The NIH HLBI Institute http://www.nhlbi.nih.gov/health/public/sleep/index.htm
The American Academy of Sleep Medicine http://www.aasmnet.org/Links.aspx
National Sleep Foundation http://www.sleepfoundation.org
Sleep Medicine Home page: An exhaustive listing of Sleep Sites http://www.users.cloud9.net/~thorpy/ Information on sleep in children for parents and physicians from the NIHLBI http://www.nhlbi.nih.gov/health/public/sleep/starslp/
Narcolepsy http://www-med.stanford.edu/school/Psychiatry/narcolepsy/ http://www.narcolepsynetwork.org